The Injury
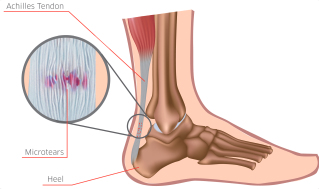
The Achilles tendon and plantar fascia are energy-absorbing and energy-releasing structures that are working throughout each stride. They absorb the load as your foot impacts the ground (loads are often 3 times your body weight) and convert the energy to propel yourself during the push-off phase of a stride (where forces are as high as 7 times your body weight).
The Achilles tendon and calf muscle are therefore an essential unit, critical for efficient and effective running. The Achilles tendon is prone to overuse purely by the nature of its function.
Pain occurs because of weakness or dysfunction in the tendon rather than what was previously thought to be an inflammatory reaction. This can be a challenging area to treat due to the tendon’s poor perfusion (blood flow), which may need longer recovery periods, so it’s best to tackle this injury at the earliest point possible.

The Symptoms
- Pain close to the heel, which is often sharp, poking and incapacitating.
- Pain along the Achilles tendon, at the back of the lower leg.
- Occasionally there can be mild swelling at the base of the tendon (near the heel) and redness.
- If you pinch the Achilles and it’s very sore, then the source of the problem is likely to be the tendon.
- Pain during and after running (Stop! This is not an injury you can run through)
- In chronic cases there can be thickening or a thickened ‘lump’ along the tendon, especially when compared to the uninjured leg.
The Cause
The Achilles tendon is the extension of the calf muscles, gastrocnemius and soleus, where it attaches to the back of the heel and is responsible for plantarflexion (pointing your toes). Sometimes excessively tight, weak calves are the culprit.
Tight lower legs put added strain on the Achilles tendon, and over the course of many months of hard training, this overuse injury can develop. A weak posterior chain (the muscles that work together along the back of your body including the back extensors, gluteus muscles, hamstrings, calves) can also be a cause of Achilles tendinopathy.
Constantly running on hard surfaces like concrete or asphalt can contribute to developing Achilles tendinopathy as the loads absorbed by the tendon are greater than running on grass or dirt roads.
Rapid increase in volume and/or intensity or training can have the same effect much more quickly, so it’s important to pay attention to both your feet and your sessions—especially when you’re training hard. Severe pronation, foot instability, a leg- length discrepancy and muscle asymmetries can also contribute to Achilles pain.
The Fix
Rest, icing, and strapping can relieve symptoms in the early/acute stages. Reducing training intensity and volume most likely will be required, possibly even complete rest for a few weeks depending on pain and the severity of the injury.
The earlier you get treatment the shorter your time off running in the ‘long run’. Soft tissue massage can be used to release tight structures throughout the lower limb and back. Physiotherapy treatment will mobilise tight structures, and prescribe rehab exercises to strengthen your calves, hamstrings, glutes and core.
Stretching along the posterior chain, such as the hamstrings is also a key component to rehab but avoid stretching the Achilles tendon in the early stages.
Advice about your shoes, orthotics and running technique can also help. Importantly, keep an eye on your training. Don’t do too much, or go too hard, too quickly.
The Prevention
When people experience Achilles tendinopathy, it often starts as a simple feeling of stiffness
in the tendon. If you take steps to increase flexibility, strengthen the ankle and calf muscles and decrease stress on the tendon at the first sign of stiffness, it’s possible to prevent the problem from escalating.
One of the easiest ways to prevent Achilles tendinopathy is to keep the tendon strong
and flexible. Regular strengthening of the calf, will be beneficial, along with a regular stretching programme.
It is important to strengthen the entire limb from the pelvis, core, hip, gluteus muscles
and hamstrings as these will all ensure the entire kinematic chain is working efficiently and minimising overload of the Achilles tendon. Then address any underlying risk factors (like shoes, orthotics) and finally a key prevention strategy is monitoring your training capacity. Slow and steady wins the race!
Rehabilitation Programme
This programme has specific exercises for Achilles Tendinopathy. Remember the key is to strengthen the calf muscle and tendon, whilst maintaining good flexibility; and don’t forget the rest of your leg! It is important to ensure the exercises are performed with good technique and good postural control. Make sure to repeat the same number of exercises on both legs.
Make sure the exercises are pain-free or minimal pain and take care not to progress too quickly. We have given suggested sets and repetitions but you can adjust these accordingly depending on pain and fatigue levels. The exercise routine should be performed twice a day.
Remember everyone is different so your therapist may give guidance that is more specific to you.
Warm up and Cool Down
If muscles are tight, weak or injured, it is particularly important to warm up (unless advised otherwise by your practitioner) with a brisk walk or a gentle jog at a pain-free pace for 5 minutes before you start your exercises. This increases your circulation and helps prepare the muscles for the activity to come. When you have finished your exercises, end the session with a 5 minute gentle walk or slow jog to allow your heart rate to slow down gradually.
Exercises
Single leg calf raise – straight knee
Stand upright on one leg. Slowly raise up onto your toes, and control the movement back down. Hold on to a wall or table for support. This exercise will strengthen the calf muscle and ankle joint.
Perform 3 x 15

Single eg calf raise – bent knee
Stand up with your knee bent, and rise up onto your toes and hold. Slowly control the movement back down. This is a strengthening exercise for the soleus (lower calf) muscle.
Perform 3 x 15

Single leg Romanian deadlift
The Romanian dead lift. Standing with your feet shoulder width apart, extend one leg behind you as you bend forwards. Soften your knee slightly, and make sure you keep your back straight (or just slightly arched) throughout the movement. When you reach horizontal, come back up to the start position (on one leg).
Perform 2 x 20

Bridge
Lie flat on your back, with your knees bent, squeeze your bottom muscles and lift your body upwards. Keep your arms by your side and use them to help you balance. Make sure you maintain good posture (do not over-arch your lower back) and contract the deep abdominal muscles by squeezing your tummy towards your spine. This exercise helps to strengthen the abdominal, lower back, gluteal and hamstring muscles.
Repeat 3 x 20

Hamstring Stretch
Lying down on your back, and bend your hip until you can feel a stretch behind your thigh (in the hamstring muscles). Use a towel to apply some overpressure and create a stronger stretch.
Hold for 20-30 secs. Repeat 3 times

Please note: The information contained in this article is intended as general guidance and information only and should not be relied upon as a basis for planning individual medical care or as a substitute for specialist medical advice in each individual case. If in any doubt or your require a more tailored programme please consult with a qualified Physiotherapist.

